Dear Healthcare Professionals,
You are incredible. You are fighting for us all. I wanted to put together a research-backed post with the best therapeutic communication techniques you can use to overcome some of the challenges you are facing right now:
- Mask-to-mask communication
- Social distancing
- Heightened anxiety
- Burnout
I had the pleasure of sitting down with Dr. Kofi Essel, my former Emory University classmate and friend! We discussed bedside manner and how to implement different rapport-building techniques, even after current this current global problem.
How can healthcare workers bond and build trust with patients? Learn from Dr. Essel and his amazing knowledge:
You can absolutely connect with your patients, even with face masks and social distancing!
I’m here to show you how. But first of all, I would like to say…
First, we have to talk about two important terms:
What is Therapeutic Communication?
Therapeutic communication is defined as an interaction from a healthcare professional to a patient and aims at promoting the physical and mental well-being of the patient. The interaction typically involves both verbal and nonverbal communication from the healthcare professional to convey a message in a calm manner.
What is Bedside Manner?
Bedside manner is the way in which a healthcare professional conveys him- or herself to the patient. Bedside manner includes factors like attitude, friendliness, and empathy. Bedside manner is one of the most important factors in therapeutic communication.
In other words, all healthcare professionals have a way in which they demonstrate their bedside manner—and it can be either good or bad depending on the person. But not all healthcare professionals have good therapeutic communication skills.
Here are my top therapeutic communication techniques to become an expert medical empathizer and spread the kindness.
Smile With Your Eyes
Ok, so here’s the hard news: A 2013 study found that doctors were perceived to be less empathetic when they wore face masks.
Ugh. Nonverbal communication with patients is hard enough, but now we have to find a way to build empathy AROUND a mask because it’s essential.
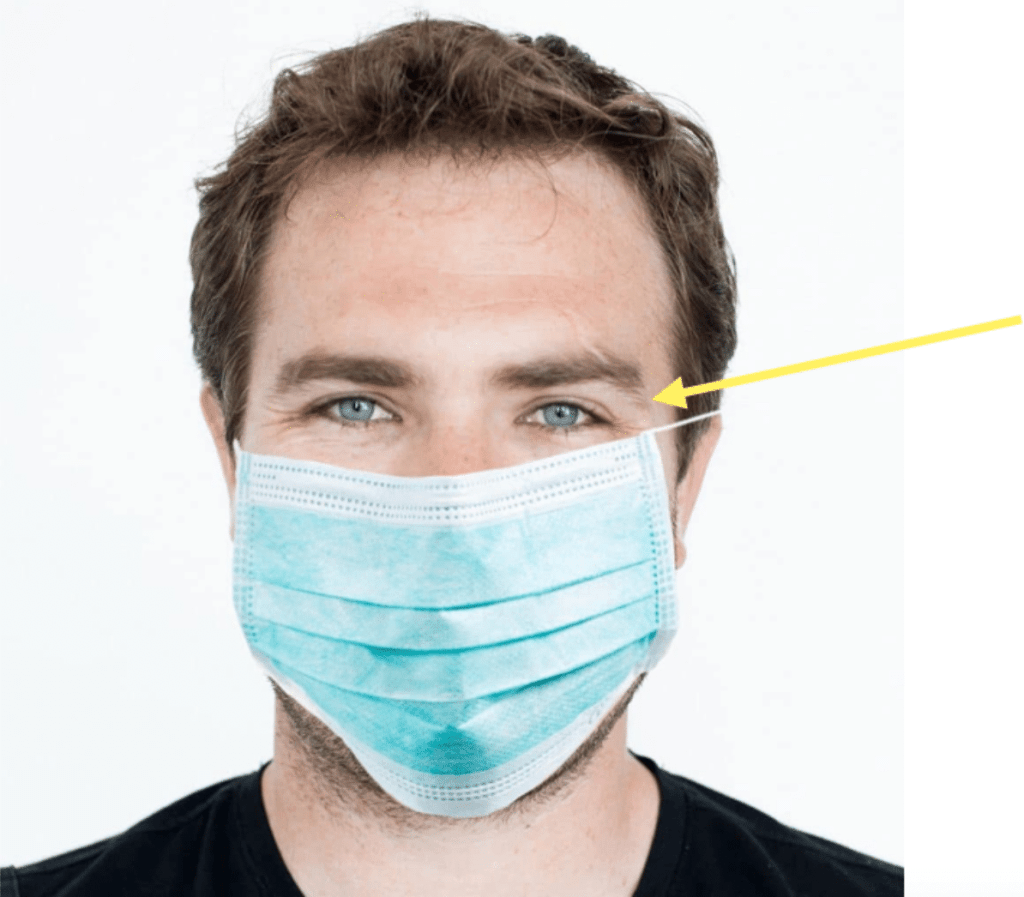
Facial expressions can be extremely hard to read with a mask on, especially if you’ve got a mask and protective eyewear on.
But there’s the good news! The old quote, “the eyes are the windows to the soul“ is actually true after all! Instead of relying on your entire face to convey your emotions, try using your eyes… not just your eyes. Your crow’s feet.
For example, even with a face mask on, patients can still see the crow’s feet wrinkles around the eyes during a genuine smile!
Be sure in the first few minutes of an interaction to smile all the way into your eyes and make sure your patient (and their support team) sees it. Dr. Barbara Wild found that we “catch” happier emotions when we see a genuine smile.
You can also display other emotions using just your eyes, such as surprise or sadness. You can learn more about how to show a genuine smile and other emotions under a mask here.
Pro tip: If you’re wearing protective eyewear, try to position yourself so there’s no or minimal glare covering your eyes so your patient can easily see you especially during the first impression.
Greet the Child
The first thing Dr. Essel does when entering a patient’s room is greet the child, if there is one. Why? Because when you make the child feel happy and show that you can build rapport and trust with them, it takes a huge load of stress away from the parent or guardian.
Put it differently, in a room with parents and a child, the doctor is the teacher, the parents are the observers, and the “child” is the student. The parents want to know their child is in “good hands,” and that can be achieved when the child is taken care of.
High fiving, elbow-bumping, asking their name, and generally engaging with them are all ways to engage with children, as well as bending down (we’ll cover that below).
Ask Open Questions
“What are your symptoms?” “Fever and headache”
“Do you need anything?” “No.”
“When did you start presenting symptoms?” “7 days ago.”
Sometimes our interactions with healthcare workers can feel like a rapid fire interview—and this is important to get to the bottom of an illness, but try to have the first or last question be more open-ended.
And it all starts with asking the right type of questions.
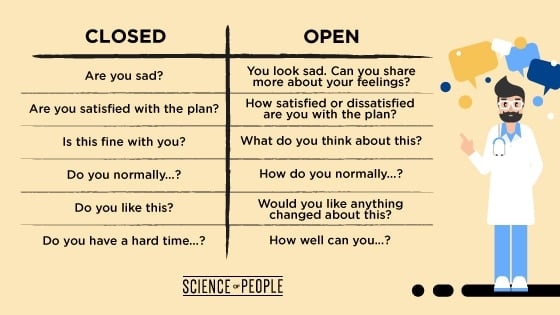
In a study of 1,527 medical students, medical interviews that lasted 5 minutes long were conducted with standardized patients.
In those 5 minutes, researchers found that patients who were asked more open-ended questions provided more information than patients in interviews with less open-ended questions!
Instead of using close-ended questions, try using open questions for better patient rapport!
Close-ended questions, on the other hand, are questions that only have one answer, either a yes or no. But not all of them are bad!
Closed questions are GREAT if you need to get a specific answer, such as if you’re asking about a patient’s background history or medicine usage, or if you’re clarifying an important date or number the patient said (if you want to be even more effective in your communication, combine this with Tip #5!).
But otherwise, close-ended questions should be used sparingly if you want to build rapport with your patient.
To avoid the above scenario, use open-ended questions.
Open-ended questions help build trust and deeper connection compared to close-ended questions. They are great as a therapeutic communication technique because they allow patients to have greater freedom to open up and talk more about what’s on their mind… instead of just saying yes or no.
Pro tip: Try closing or opening on a standard open-ended question you like. For example, “Anything else you want to tell me?” is a great one. You might also ask these kinds of questions to family members that are with your patient.
The Triple Nod + Head Tilt
One of the most powerful therapeutic communication techniques is called the triple nod. And the best part: this works with a mask!
A 2017 Japanese study published in the psychology journal Perception studied the effects of nodding on attractiveness:
- They asked 49 adults to watch computer-generated video clips of figures nodding, shaking their head, or staying still.
- The participants then rated the figures’ attractiveness, approachability, and likability.
The results?
Nodding figures were rated 30% more likable and 40% more approachable than figures that shook their head or were motionless.
And if nodding makes you more likable and approachable, don’t just nod once.
Instead, try the triple nod when you want someone to open up.
The triple nod is like a nonverbal… ellipses.
It says:
- Keep going…
- Tell me more…
- What else…
I love the triple nod for showing empathy and good bedside manner.
Warnings:
- Be sure this is a SLOW triple nod. A fast triple nod signals more impatience.
- Don’t bobblehead! Only use the triple nod when you want someone to open up, or you want to show that you agree.
Remove All Barriers
Dr. Essel mentions that he will remove all barriers, such as computer desks, between him and the patient. In the world off body language, having barriers in place means effectively blocking yourself from your patient.
It’s basically a subtle “arms crossed” gesture.
What Dr. Essel does, instead, is he turns his body and engages with his patients with his torso turned towards them, but also makes sure to keep notes on his computer by typing off to the side.
When a patient is sharing something deep or really concerning, Dr. Essel will stop typing and turn his full body towards them, giving them the time and attention they need.
Get on the Same Level
Humans have this weird instinct: we do not like it when people hover over us. Have you ever had someone hover and peek over your shoulder? Or stand and talk to you while you were sitting? It doesn’t feel great. ESPECIALLY during a first impression.
Research published in the Patient Experience Journal shows that nurses who sit down when communicating with patients received a higher patient satisfaction rating. More specifically, the researchers found that at the end of the 7-month study, nursing communication and satisfaction scores in the Texas hospital they conducted the study rose from the 9th percentile to the 43rd percentile.
On a personal note, here’s a good example that happened just yesterday:
I was out on a walk with my 2-year old Sienna when I ran into an old colleague of mine (let’s call him Jim). Jim was excited to see Sienna since we haven’t seen each other in a while, and he stood there asking questions to her like “When was the last time you watched Frozen?” and “What’s your favorite food?”
What was his mistake?
Now Jim’s a great guy, but he simply wasn’t standing at the same level as her. He was literally covering Sienna with his shadow during our entire conversation!
Don’t stand over or hover above patients; kneel down and get to their height if you have to… especially during a first impression.
I have spoken to many dental groups and always suggest that they come in the room and take a seat on the stool immediately while they greet their patients. I have heard great results from this simple tip!
Remember: Slide into that stool.
Especially if your patient is a younger child or elderly individual. This shows you care and lets the patient feel a lot less intimidated when you’re talking to them. Patients can also read your eyes better to read your emotions.
Upgrade Your Communication Toolkit
Imagine this: a patient has been diagnosed with a chronic disease. You are designated as the comfort giver. What do you say?
- Everything will be OK.
- I’m sorry to hear that.
- I hope you get better.
- Life is really tough sometimes.
How about none of the above? Having just the right comfort phrase during difficult situations can make a world of difference for your patient when he or she is suffering.
So if you’re running out of things to say, perhaps you need to upgrade your therapeutic communication toolkit.
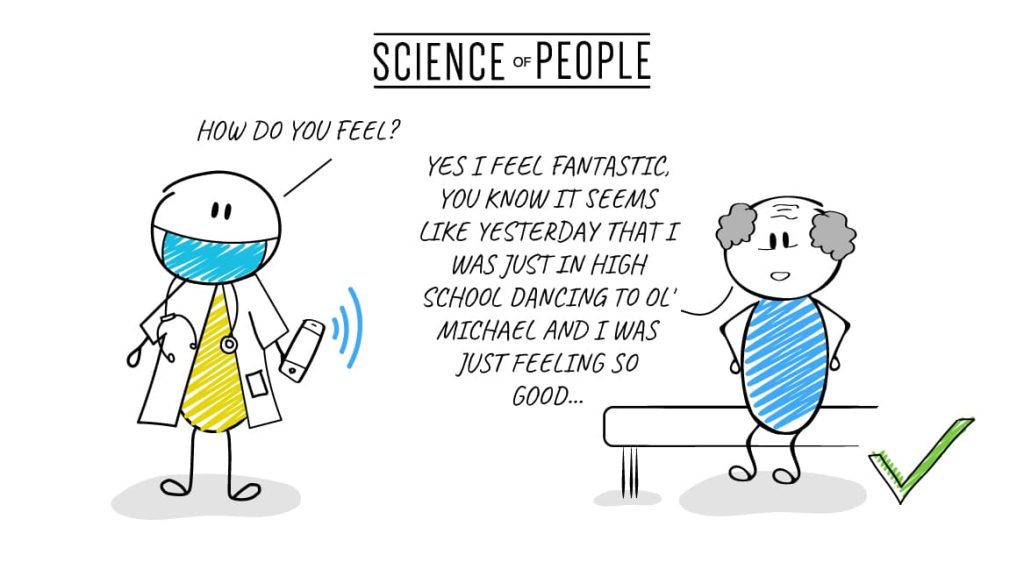
For example, a 2012 study found that people who disclosed a personal bit of information were perceived as more likable and positive than those that just listened to others.
Successful phrases or questions fall into one of these 7 categories:
- Restating: Repeating the patient’s exact words in order to clarify or gain more information
- Reflecting: Turning the focus back to the patient to gain more intel on a situation

- Paraphrasing: Restating a patient’s story in a shorter manner to confirm what you think you just heard
- Exploring: Allows you to gather more information about something that the patient has just mentioned

- Leading: A question or statement to allow the patient to guide the discussion
- Presenting Reality: A statement or question that presents something “as is” rather than trying to make a situation seem better off than it actually is
- Self-Disclosing: Sharing something about your personal life or self and then turning the focus back on the patient. This helps build trust and rapport
Here are also 3 things you MUST avoid to communicate effectively:
- “Why?” Questions: Asking why questions can often lead to a patient being provoked or feeling angry / upset.
- Opinions: Offering advice that is based on speculation or personal experience

- Toxic Positivity: Saying something will turn out OK when it won’t

The next time you’re trying to build rapport with your patient, try implementing one of these 7 phrases, and avoid the 3 harmful ones!
The Pen is Mightier Than the Mouth
Good communication in nursing or healthcare shouldn’t rely on just the voice. When voice isn’t an option, try good old-fashioned ink on paper.
I highly recommend carrying a handy little notebook and pen with you, if you don’t already. This makes it easier for you to jot down important dates or facts that you want to clarify with your patient.
And if you think it’s rude— think again! Have you ever given an order to a waiter or waitress, and they stand there nodding while you and your family or friends spit rapid-fire orders at them? Seriously! How do they even memorize that?
Taking down notes makes you appear more considerate and makes your patient feel like what you’re saying matters.
And a great way to get your patient on board with the writing process is to use a digital writing tablet! They’re fun to use, easy to write with, and can be used over and over again.
Special Tip: Taking notes about how their life at home has been is a great way to connect with patients. You can review your notes (if any) before going into a patient’s room and recall personal information about them— ie. “How was the baseball game?” This is a great tip to boost your patient-bonding and makes them feel like you care.
Lower Your Pitch
Heavy, hard-to-breathe-in N95 masks can be difficult to hear in, especially if you’re keeping distance or your patient has a hard time hearing.
Here’s what NOT to do: Shout.
Here’s what to do instead: Use a low vocal pitch.
When speaking with a lowered pitch, you’ll come across as clearer and easier to understand, thus building better rapport with patients. A lower voice is also just really nice to listen to.
Vocal coach, Roger Love explained to me that going lower in your range saves your voice and makes you more clear. Watch that interview here:
Pro tip: Don’t go below your vocal range. Find your natural vocal range in our article here.
Your Joke Arsenal
Laughter truly is the best medicine. It’s also one of the best therapeutic communication techniques.
Laughter has even been scientifically proven to decrease stress hormones and increase antibody production in the person laughing. Therapeutic humor is especially helpful for patients who are coping with a difficult illness.
Along with comfort phrases, adding in a little humor is an amazing way to make your patients feel better.
The only thing you should be aware about is to use your own judgment when it comes to being offensive or not, and avoid anything political, racial, or cultural. A good rule of thumb is if you wouldn’t tell a little kid this joke, don’t use it!
For a funny example, here is a funny knock-knock joke you can watch from Yours Truly:
If you’re not naturally funny or you’re a recovering awkward person like me, try building up your humor by studying your favorite standup comedians or reading my article on how to be funny.
Encourage After-Activity
Empathy in healthcare shouldn’t just stay in the hospital.
If your patient is clear and ready to leave, you can help by encouraging them to take up an activity or learn a new hobby during social distancing.
The fact is, many people who come back from the hospital or doctor’s office are living alone or unemployed. A television, bed, and sofa might be all they have when they return home, and going back only to spend their time idly watching television or spending time alone can be a drain on their mental health.
A great aftercare therapeutic communication technique is taking a few minutes out of your day to make sure your patient has something to do with their idle time when they return home. And if you can help them stay connected socially— even better!
Science says connecting socially and making friends is one of the best ways to a longer, happier life.
Prepare for Virtual Calls
A video call is one of the most effective ways to communicate with a patient’s family and loved ones whenever a patient needs to stay overnight.
And if you’re not a fan of video calls, there are ways to make them better for both you and the patient!
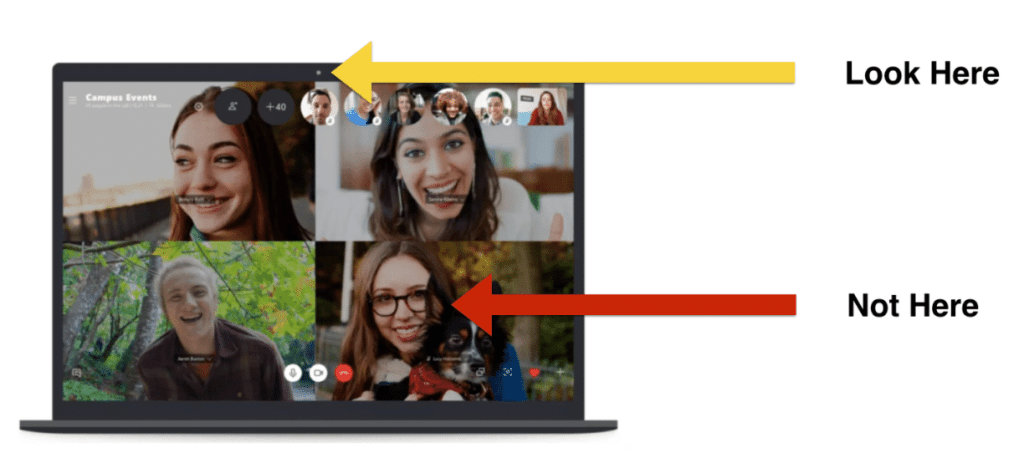
For example, one excellent tip that comes from our video calls article is to look at the dot or camera, not the screen! Why?
According to a 2014 study by researchers from the UK’s Medical Research Council:
People who receive direct eye contact with others appear to activate a certain part of their brain called the “social brain” network.
What is the “social brain” network? It’s the part of the brain that allows us to have genuine social interaction. When the social part of your brain lights up, you can tell jokes, have fun, and smile without faking it.
But this only happens if you look at the camera… NOT at yourself.
Talk to Your Phone
No matter how many times you’ve done it, sometimes talking to patients while trying to write down information is an impossible task:
Whether your patient is a fast talker or you simply have a lot of information coming your way, one great therapeutic communication technique is to try is speech-to-text software.
What is speech-to-text software?
According to techopedia, speech-to-text software is a type of software that effectively takes audio content and transcribes it into written words in a word processor or other display destination.
Some speech-to-text software can even detect voices from several feet away, making this a great way to free up your hands and pay 100% focused attention to your patient.
Speechnotes is a free one you can try. There’s even a medical-based speech-to-text software you can use! Alternatively, you can use the voice recorder app on your phone to capture now and write later.
Pro Tip: If you are taking notes, be sure to pause and look up during your questions to make some eye contact.
Wear a Clear Face Mask
I know this isn’t an option for everyone, but a way to demonstrate great therapeutic communication techniques to your patient (and even create loads of laughter!) is to wear a face mask with a clear rectangle to show your mouth.
This is exactly what a senior from Eastern Kentucky University did to help people who are deaf and hard of hearing pick up on facial cues:
INCLUSION MATTERS: A college student, Ashley Lawrence, makes mask for the deaf and hard of hearing with a plastic window so they can still communicate. https://t.co/qew66ABWJJ
— COVIDPROMISE (@covidpromise) April 13, 2020
Other manufacturers of similar masks include Safe ‘N’ Clear and ClearMask. #CovidPromise #covid19 pic.twitter.com/svd06YMVO4
And there are already companies offering face masks with clear smile slots like ClearMask and Safe ‘N’ Clear!
You Are a Hero
As someone who personally knows individuals who have been affected by recent events, I want to say thank you. You have truly made a big impact during this time, and this article is for you!
You are my hero!
I hope you added some knowledge to your therapeutic communication technique arsenal!
Without your help, the world would be in a dangerous place.
From the bottom of my heart, I just wanted to say…
You are AMAZING!
Thank you!
Sincerely,
Vanessa
Crack The Code on Facial Expressions
The human face is constantly sending signals, and we use it to understand the person’s intentions when we speak to them.
In Decode, we dive deep into these microexpressions to teach you how to instantly pick up on them and understand the meaning behind what is said to you.
Don’t spend another day living in the dark.
Vanessa,
I have been following you for the past 2 years and you are always on point. Today you pointed out that I am a real hero. I never thought of myself like this. I always thought I was doing what I signed up for by choice. When COVID happened I volunteered to take care of patient;s in the ICU while others ran. Thank you for your words.
Vanessa,
I have been following you for the past 2 years and you are always on point. Today you pointed out that I am a real hero. I never thought of myself like this. I always thought I was doing what I signed up for by choice. When COVID happened I volunteered to take care of patient;s in the ICU while others ran. Thank you for your words.
Vanessa,
I have been following you for the past 2 years and you are always on point. Today you pointed out that I am a real hero. I never thought of myself like this. I always thought I was doing what I signed up for by choice. When COVID happened I volunteered to take care of patient;s in the ICU while others ran. Thank you for your words.
Vanessa,
I have been following you for the past 2 years and you are always on point. Today you pointed out that I am a real hero. I never thought of myself like this. I always thought I was doing what I signed up for by choice. When COVID happened I volunteered to take care of patient;s in the ICU while others ran. Thank you for your words.